The 2025 residency match exposed a scandal: 10,000 qualified American medical graduates left unmatched, their dreams deferred by a system that prioritizes foreign-trained doctors over its own. But this crisis is no aberration—it’s the culmination of a decade-long betrayal. Over the past 10 years, from 2015 to 2025, an estimated 25,000–35,000 U.S. allopathic seniors have been excluded from residency programs, exacerbating a physician shortage projected to reach 124,000 by 2034, per the Association of American Medical Colleges (AAMC). Meanwhile, 75,000 foreign-trained doctors—international medical graduates (IMGs)—secured taxpayer-funded residency positions,paid for by Medicare’s graduate medical education (GME) funding, totaling $11.25 billion–$15 billion over the decade. The American Medical Association (AMA), accused of artificially limiting residency slots, and the influx of IMGs on J-1 visas have created a bottleneck that White-Collar Workers of America decries as yet another front in the war against American workers. Let’s uncover the staggering cumulative impact, the systemic failures driving it, and why it’s time to act.
The Data: A Decade of Unmatched Doctors
The residency match, facilitated by the National Resident Matching Program (NRMP), has consistently left American medical graduates in limbo. In 2015, 41,334 applicants registered for the Main Residency Match, with 30,212 U.S. allopathic seniors submitting rank lists, per Web ID 2 (MedEdits). Of those, 93.9% (28,358) matched, leaving 1,854 unmatched, according to NRMP statistics. Over the years, applicant numbers rose to 48,156 by 2023, but residency slots grew minimally, from 35,185 in 2019 to 38,000 in 2025, per Web ID 1 (AMA).
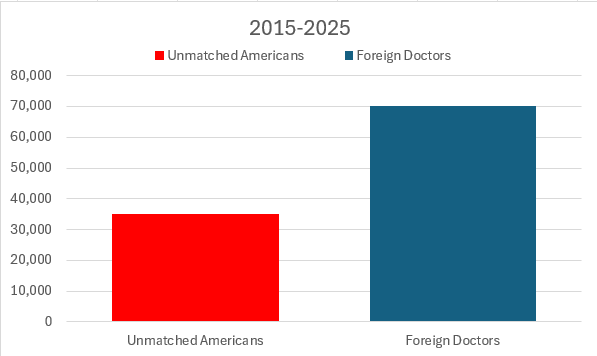
Assuming a 5-7% unmatched rate for U.S. seniors (based on historical NRMP data), and with 27,000–28,000 U.S. seniors annually, the cumulative number of unmatched U.S. allopathic seniors over 2015–2025 is approximately 25,000–35,000. This figure includes only U.S. seniors, not osteopathic students or IMGs, and does not account for re-applicants. Meanwhile, over the same period, 75,000 IMGs matched into U.S. residency programs, per NRMP data and AAMC estimates. These slots, funded by Medicare’s GME program at $150,000–$200,000 per resident over three years, cost taxpayers $11.25 billion–$15 billion, highlighting a stark disparity: for every unmatched American graduate, roughly 2–3 IMGs secured a taxpayer-funded position, displacing American talent.
The Human Cost: Lives and Careers Derailed
For these 25,000–35,000 American doctors, the impact is devastating. Each unmatched graduate carries an average student loan debt of $200,000–$300,000, per the AAMC, and faces a future without a medical license, as residency is required to practice. Many pivot to non-clinical roles—consulting, research, or administration—but this represents a tragic squandering of years of training. Others endure the emotional toll of rejection, reapplying year after year or leaving medicine entirely. X users like @unmatchedmd have voiced this frustration,
The ripple effect extends to patients. With a physician shortage projected to hit 124,000 by 2034, per Web ID 0 (AAMC), the loss of these American doctors deepens rural and underserved area deficits. Family medicine, a critical need, sees thousands of unmatched American graduates annually. Web ID 3 (PMC) shows family medicine’s fill rate for U.S. seniors dropped to 33.2% in 2020, with many slots filled by IMGs, leaving American talent untapped.
The AMA’s Role: A Decade of Deliberate Restriction
The AMA’s fingerprints are all over this crisis. Over the past decade, the organization has maintained its historical stance on limiting residency slots, rooted in the Balanced Budget Act of 1997, which froze Medicare funding for graduate medical education (GME) at 1996 levels. Web ID 1 (AMA, 2024) notes that Congress has failed to expand these slots, despite proposals like the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 positions over seven years. The AMA, while advocating for more slots publicly, has resisted rapid expansion, citing quality concerns—a position that White-Collar Workers of America sees as a pretext to protect the profession’s elite while sidelining American graduates.
This policy has directly enabled the displacement of American doctors by IMGs, as the limited slots are filled by foreign-trained physicians funded by taxpayers, while U.S. graduates are left unmatched.
Foreign-Trained Doctors and Taxpayer Funding: A Decade of Displacement
The influx of 75,000 IMGs into U.S. residency programs over 2015–2025, funded by $11.25 billion–$15 billion in taxpayer money through Medicare GME, has worsened the crisis. Many of these IMGs enter on J-1 visas, per Web ID 3 (Wikipedia), which are designed for cultural exchange but often lead to permanent U.S. residency, competing directly with American graduates for slots. A 2021 National Bureau of Economic Research study found that IMGs now constitute 25% of the U.S. physician workforce, their residency training subsidized by American taxpayers while U.S. doctors shoulder $200,000–$300,000 in debt without a path to practice.
White-Collar Workers of America, known for its fight against H-1B and J-1 visas in tech and other fields, sees this as a parallel betrayal. The website emphasizes protecting American jobs from foreign labor, arguing that these visa programs undercut U.S. wages and displace domestic talent. In medicine, IMGs on J-1 visas occupy taxpayer-funded residency slots, leaving 25,000–35,000 American graduates unmatched over a decade—a ratio of 2–3 IMGs per unmatched American, a stark indictment of a system that prioritizes foreign labor over American talent.
The Economic and Social Toll
The cumulative impact of 25,000–35,000 unmatched doctors over a decade is a national tragedy. Economically, it represents a $5 billion–$10 billion loss in human capital, assuming each unmatched doctor’s education cost $200,000–$300,000 and their potential earnings as physicians (averaging $300,000 annually, per Medscape) are forgone. Socially, it exacerbates healthcare disparities, leaving rural and underserved areas without needed providers. Web ID 0 (AAMC) projects primary care shortages of 55,000 by 2034, a gap widened by the failure to match American graduates in family medicine.
Inflation fears also loom, as these displaced doctors compete for non-medical jobs, driving down wages in other sectors. The tight labor market, with unemployment at 4.1% in February 2025, per the Bureau of Labor Statistics, means their skills are underutilized, potentially increasing wage pressure and consumer prices, per Web ID 1. Meanwhile, the $11.25 billion–$15 billion spent on IMGs’ residencies represents a misallocation of taxpayer funds, subsidizing foreign labor while American doctors are left behind.
A Call to Action: End the Betrayal
This decade-long crisis demands action. White-Collar Workers of America calls for an immediate expansion of residency slots—doubling Medicare-funded GME positions to match medical school output—and a moratorium on foreign-trained doctors on J-1 visas until every qualified American graduate is matched. Congress must pass and fund the Resident Physician Shortage Reduction Act, but it’s not enough; we need a 50,000-slot increase over five years to meet the AAMC’s projections.

